November 4, 2025
AI is transforming insurance claims by making the process faster, simpler, and more reliable. Embedded insurance integrates coverage directly into platforms people already use, like apps or websites, making it easier to file claims without switching systems. When combined with AI, this approach automates tasks like verifying claims, analyzing damage, and detecting fraud, reducing resolution times from days to minutes.
Here’s what you need to know:
This shift benefits customers with faster, transparent claims and helps insurers cut costs, improve efficiency, and build loyalty. Learn how these advancements are reshaping the insurance experience.
The shift from traditional claims handling to embedded insurance claims processing has completely reimagined how claims are managed. Three key factors drive this transformation: automated API integrations, digital cost efficiencies, and no-code management tools that are easy to use and implement.
API-driven claims integration is at the heart of the embedded insurance model, creating a smooth connection between customer actions and insurance responses. For example, when a claim is filed through an embedded platform, APIs instantly verify eligibility using real-time data. This real-time integration also strengthens fraud detection and risk assessment, ensuring claims are processed both quickly and accurately. By automating these steps, insurers can significantly cut operational costs while improving efficiency.
Switching to digital processes offers major cost savings across various operational areas. Automated workflows reduce administrative overhead by minimizing manual tasks and ensuring compliance with built-in audit trails. Faster claim cycles also mean fewer customer service interactions, which lowers associated costs. These digital systems free up resources, allowing insurers to focus on improving customer satisfaction. On top of that, no-code tools make it even easier for SaaS platforms to streamline their claims processes.
No-code claims management tools are a game-changer for non-technical teams, enabling them to design, build, and refine claims workflows without needing to write a single line of code. These platforms allow for rapid deployment and adjustments, cutting development times by up to 60% compared to traditional systems [1] [2]. They also make it simple to experiment with and optimize claims processes in real time, giving businesses the flexibility to adapt quickly and scale efficiently.
Claims automation in embedded insurance takes the headache out of traditional claims processing. By replacing manual, paper-heavy methods with a streamlined, automated approach, it transforms what used to be a frustrating experience into one that’s smooth and efficient. When claims are resolved quickly and transparently, customers feel reassured about their coverage. Let’s explore how simple initiation and clear updates enhance every step of the claims journey.
Gone are the days of juggling multiple platforms or waiting endlessly for updates. With embedded insurance, customers can file claims directly within the apps or platforms they already use - whether it’s a ride-sharing app, an e-commerce site, or a travel booking service. This means they can report incidents, upload photos, and track progress without ever leaving their familiar digital environment.
The resolution process is just as seamless. Automated systems instantly verify eligibility, and straightforward claims are often approved and paid within minutes. For instance, imagine a ride-sharing app user with embedded insurance who damages their phone during a trip. They can report the issue, upload photos, and get approval for replacement costs - all within the same app they use every day.
Real-time updates further enhance the experience. Instead of chasing down information, customers receive notifications at every step, keeping them informed and eliminating the stress of uncertainty. This level of communication not only saves time but also builds trust.
Embedded insurance systems take personalization to the next level by leveraging customer data. These systems already know coverage details, purchase history, and preferences, allowing them to tailor communication for each claim. This creates a claims process that feels intuitive and relevant to the individual.
Transparency is another game-changer. Customers can track their claim status at any time, seeing exactly when documents are received, when reviews are underway, and when payments are processed. This level of visibility removes the guesswork and anxiety that often come with traditional claims processes.
To make the experience even smoother, updates are delivered through the customer’s preferred communication channels - whether it’s email, text, or in-app notifications. This thoughtful approach ensures that the process feels both efficient and considerate.
Fast, fair, and reliable claims resolution directly impacts how customers perceive their insurance provider. When claims are handled smoothly, it reinforces trust and strengthens the relationship between customers and insurers.
For businesses, the benefits go beyond immediate satisfaction. A seamless claims process encourages repeat purchases, generates referrals, and fosters long-term loyalty. Platforms offering embedded insurance gain a competitive edge, as these positive experiences translate into higher conversion rates and increased customer lifetime value.
Additionally, no-code claims management tools allow businesses to adapt their processes based on customer feedback. This flexibility ensures that the claims experience continues to evolve and improve, creating a cycle where better service leads to happier customers and stronger business relationships. It’s a win-win for everyone involved.
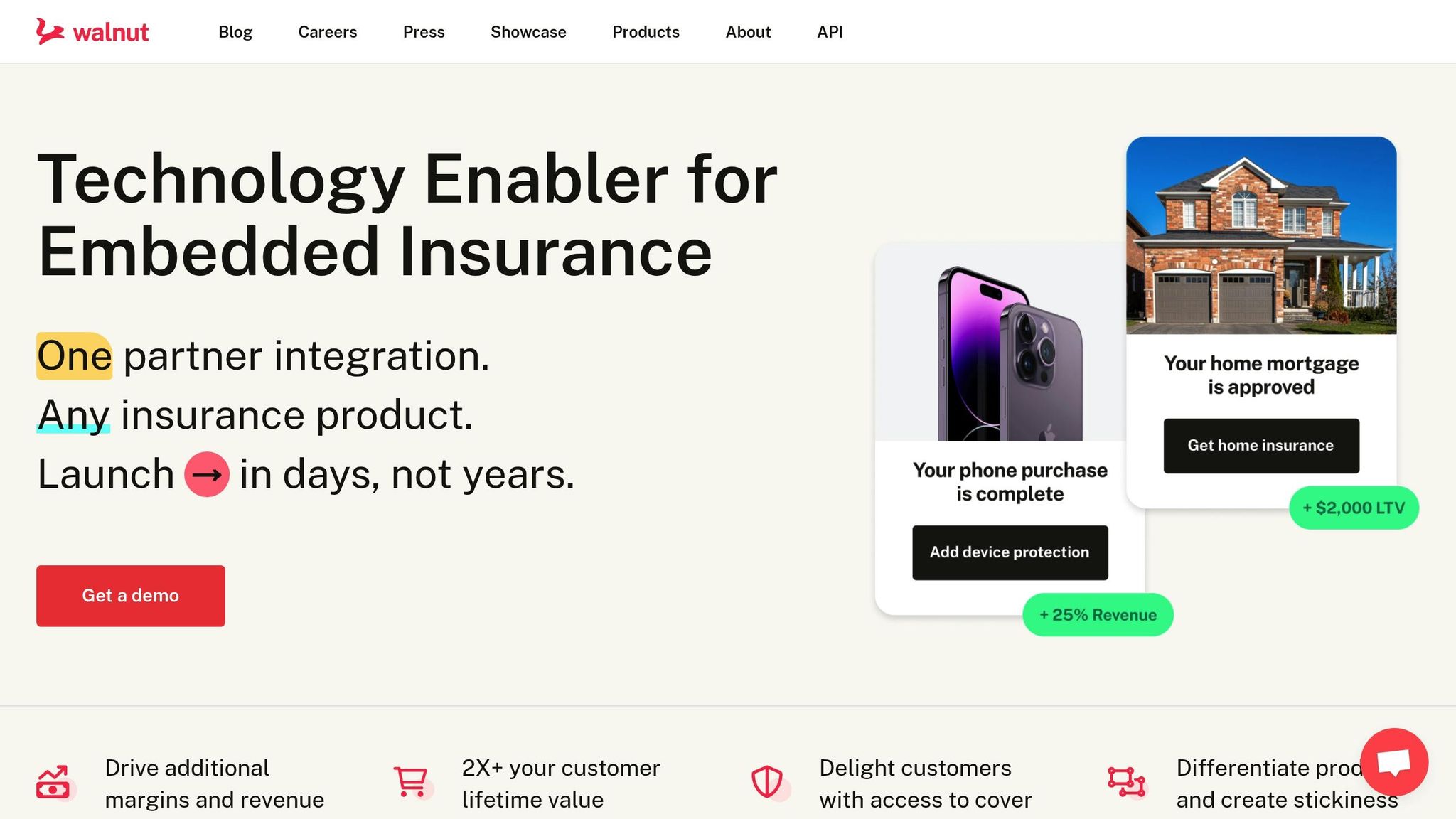
Walnut simplifies the process of handling embedded insurance claims by bridging outdated systems with modern digital workflows. This connection allows insurance providers to integrate their services with minimal complexity, paving the way for faster and more efficient claims processing.
Walnut's platform offers flexible integration options, including APIs and no-code solutions, making it easier for partners to connect with over 14 insurance carriers. This connectivity supports smooth claims processing across a variety of insurance products. Features like instant quote and bind capabilities streamline eligibility checks and policy setup, enabling businesses to create customized insurance programs. These tools work together to support AI-driven claims management that prioritizes speed and efficiency.
By automating processes, Walnut helps reduce operational expenses and improve the overall customer experience. Integrating insurance offerings directly into the core service creates a seamless experience for users, turning insurance into a natural part of their journey. This approach not only drives revenue but also strengthens customer loyalty by making the insurance process more accessible and less intrusive.
Walnut's infrastructure is designed to ensure compliance with regulatory standards across multiple channels, so partners can stay within legal boundaries without needing in-depth insurance knowledge. Deployments are typically completed in just 30 to 90 days [3][4], allowing businesses to quickly adapt to market needs and expand their insurance services across regions. Walnut also keeps solutions up-to-date with regulatory changes, ensuring businesses remain compliant as laws evolve. This combination of scalability and compliance equips businesses to meet the demands of a rapidly changing market.
Embedded insurance claims processing offers clear advantages, but implementing these systems isn’t without its hurdles. Tackling these challenges with thoughtful planning and effective strategies can help organizations create automated claims processes that enhance both customer satisfaction and operational efficiency.
While automation speeds up claims processing and boosts customer satisfaction, it also opens the door to certain risks. High-volume, low-complexity claims, in particular, can become targets for fraud, making robust safeguards essential.
Multi-layered validation is key to minimizing vulnerabilities. Automated systems must verify claim details against policy data, historical trends, and external databases in real-time. This includes checking whether the reported incident falls within the policy’s coverage period, identifying duplicate claims submitted through different channels, and flagging unusual patterns - like multiple claims originating from the same location or device.
Behavioral analytics add another layer of fraud detection by monitoring patterns such as claim submission frequency, spikes in specific claim types, or unusual user behavior. When these patterns stray from established norms, the system can flag the claim for human review. Dynamic risk scoring helps fine-tune the process, allowing straightforward, low-value claims to move forward quickly while subjecting higher-value or irregular claims to additional scrutiny.
Many insurance companies still rely on legacy systems, which can make embedding claims automation a complex task. These older systems often operate with outdated data formats, lack real-time processing capabilities, and depend on manual workflows for even basic tasks.
APIs act as bridges, enabling modern platforms to communicate with legacy systems. These interfaces translate data, handle authentication, and manage timing mismatches between real-time embedded solutions and batch-processing legacy systems. This approach allows companies to upgrade their claims processing without replacing their existing infrastructure entirely.
Data synchronization strategies are crucial for ensuring smooth information flow between systems with different update cycles. For instance, real-time embedded systems require immediate access to policy details, while legacy systems may only update overnight. Cached data layers with intelligent refresh mechanisms can provide up-to-date information without overloading the legacy infrastructure.
A phased migration approach offers a practical path to modernization. Instead of attempting a full system overhaul, companies can start by automating specific claim types or customer segments using embedded platforms. Complex cases can remain on legacy systems, reducing implementation risks and allowing teams to gradually adapt to new technologies.
Beyond technical challenges, striking the right balance between automation and human oversight is essential. Over-automation can mishandle unique or complex claims, while too much human involvement can erode the efficiency gains automation promises.
Establishing clear escalation criteria ensures consistency in determining when claims need human review. Factors like claim value, policy complexity, customer history, and the confidence level of automated assessments should guide these decisions. For instance, claims involving personal injuries, disputed liability, or high-value payouts might automatically route to human adjusters.
Hybrid processing workflows offer the best of both worlds. Automated systems can handle routine tasks like claim intake, document collection, and basic eligibility checks, while human reviewers focus on more nuanced tasks, such as resolving disputes, managing sensitive cases, and ensuring quality control. This approach maintains efficiency while preserving the trust and satisfaction that come from personalized service.
Continuous learning mechanisms allow automated systems to evolve by analyzing human reviewers’ decisions. When adjusters override automated outcomes or handle escalated cases, the system can capture these insights to refine its processes. Over time, this feedback loop reduces unnecessary escalations and improves the system’s accuracy.
Offering customer choice integration can further enhance the claims experience. Some policyholders prefer the reassurance of human interaction for significant claims, while others prioritize speed and convenience. Giving customers the option to request human review or stick with automated processing ensures the experience aligns with their individual preferences, boosting overall satisfaction.
Embedded insurance is reshaping how claims are processed, revolutionizing both customer relationships and operational workflows. By transitioning from traditional, manual claims handling to AI-powered, automated systems, the insurance experience becomes faster, smoother, and more efficient at every level.
Automation dramatically reduces the time it takes to process claims - what once took days can now be completed in minutes. With API-driven integration, filing a claim becomes a seamless experience, embedded directly into the platforms customers already use. Instead of being a frustrating chore, claims processing becomes a natural part of their digital journey.
This efficiency does more than just save time - it elevates the entire customer experience. It’s not just about speed; it’s about delivering a service that feels effortless. Features like instant eligibility checks, real-time status updates, and personalized communication create a level of service that fosters long-term loyalty. When customers can file and track claims without jumping between platforms, satisfaction rates rise significantly.
The financial upside of this transformation is just as compelling. Automating claims processing reduces administrative costs, eliminates many manual errors, and frees up staff to focus on complex cases that genuinely need human attention. These cost savings often offset the initial investment in automation within the first year. Additionally, the improved customer retention that comes with better service adds long-term value. Businesses can now offer a complete insurance experience without having to build a complicated claims infrastructure from scratch. This accessibility opens up new revenue opportunities while enhancing the overall value they deliver to customers.
Embedded insurance also enables proactive fraud management, seamless integration with legacy systems, and careful automation oversight - ensuring the system runs smoothly and securely.
Companies that see claims processing as an opportunity rather than a burden will come out ahead. Embedded insurance claims processing turns efficient, customer-focused claims handling into a competitive edge. Tools like Walnut’s API and no-code solutions demonstrate how this transformation can happen almost immediately, turning claims from a cost center into a strategic advantage.
Embedded insurance is transforming the way claims are processed by swapping out outdated, manual workflows for automated, data-focused systems. This shift introduces game-changing features like instant eligibility checks and claims automation, slashing processing times and cutting down on administrative hurdles.
With the help of AI-driven tools and APIs, claims are handled faster and more precisely, improving the overall customer experience while trimming operational expenses. This streamlined approach not only enhances efficiency but also strengthens trust, increases customer satisfaction, and encourages long-term loyalty.
No-code platforms are transforming how insurance companies adopt AI-driven claims processing. These tools remove the need for deep coding knowledge, enabling insurers to design and launch automated claims workflows that match their unique requirements - fast.
Using no-code solutions, insurers can embed AI features such as instant eligibility checks, fraud detection, and real-time data analysis directly into their claims systems. This approach not only cuts down on administrative tasks but also boosts processing speed and accuracy. The result? Insurers can offer a smooth, customer-focused claims process without the hefty expenses or delays tied to traditional software development.
AI and API-driven systems are transforming fraud detection and prevention in claims processing by tapping into advanced data analysis and automation. With machine learning algorithms, these systems sift through historical data, identify patterns, and flag unusual anomalies that might signal fraudulent activity. This proactive method not only boosts accuracy but also cuts down on cases of undetected fraud.
Beyond fraud detection, AI simplifies tasks like document validation and data entry, making the claims process faster and more reliable. For instance, optical character recognition (OCR) technology can instantly digitize and verify documents, while sophisticated algorithms evaluate damages and calculate repair costs, ensuring settlements are both fair and efficient. By automating these steps, insurers save on operational costs and can prioritize creating a smoother experience for their customers.